Hi All,
I read often, but don't post too much. I appreciate the wealth of knowledge you all have and feel grateful there is this space for those who need help, comfort, support, etc.
The reason for my post tonight is due to some "new" feelings/sensations I've been experiencing as of late, none to pleasant.
For the past 6-8 weeks, I've noticed a decline not in the quantity of BMs, but in the quality. I feel as though I have larger urges, with less output despite more pushing/straining than usual. Blood has made an appearance, though only a few times, not regularly. My normally large amount of passed gas has seemingly disappeared, leaving feelings of bloating (extremely uncomfortable). In the past, I have been able to lay face down and manipulate my body to assist in passing gas - this no longer works.
Additionally, I notice that after these dissatisfying BMs, I feel a bad sense of pain/pressure at the anal opening. I can't tell if it's internal or external, but would guess internal if I had to. This lasts for quite a while, longer if I allowed myself to sit and strain. At times, it's so uncomfortable, I can't sit. As you can guess, pretty debilitating overall.
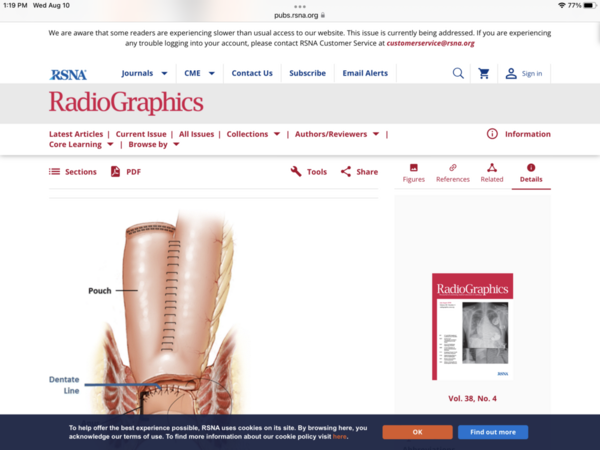
My 2-step surgery was in 2004, with only small bouts of obstruction and pouchitis over the years. My surgeon has retired and my GI moved on, so I'm waiting for my appointment with the new GI. Anyone have any suggestions for self relief at home while I wait for my October appt?
(Currently trying to do mostly liquids, Atrantil daily, Iberogast weekly).
Thanks as Always-
Ken